Hospitals speak the language of Return On Investment (RoI). When evaluating any new technology, a key criterion is the expected ROI. How many tests / procedures can be performed with the said technology? What is the useful life? What revenues can it generate?
When it comes to Surgical instruments, ROI is impossible to compute. What revenue do surgical instruments bring in? How many surgeries does each instrument last for?
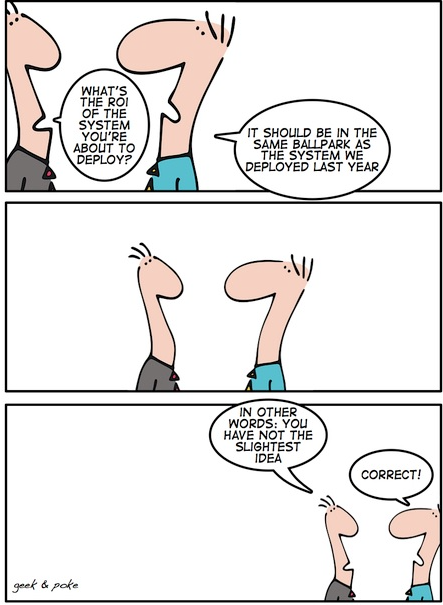
So, by extension then, what is the RoI of a Surgical Instrument tracking system? Goes without saying, the ROI for a Surgical Instrument Tracking System is even more difficult to calculate!
But then there is COI – or Cost of Inaction.
Consider this:
- If you are a 500 bedded hospital, you might carry surgical instrument inventory of 8,000 to 10,000 instruments. Today, you have no insight on the status of this asset. What is the useful value of this asset? What should be your annual replacement budget? Can you continue with status quo?
- What value will it bring to know the useful life of instruments, to track them through their life cycle?
- Turnover of nursing staff and technicians is only likely to increase. Each time a new hand takes over a manual process, there is discontinuity. And this discontinuity impacts surgeons and caregivers. What is the cost of not having a person-independent system?
- What are the hidden costs of running a manual process? We already spoke about wasted cycles and Just In case inventory here & here.
- Is this cost of inaction palatable – when you look ahead 3 years or 5 years ahead?
Surgical instruments are a revenue generating asset. The way to improve RoI is bring down the CoI by changing the way this asset is managed.

With changing technology and skill upgradation there are many surgical instruments that need to be replaced with advanced version thus it’s value will also help the hospital in negotiating for buy back option rather than outright purchase and then worrying about the obsolete inventory
Eye opener to hospital